Adaobi Lisa Olisa, Fellow, IAS 2024 HIV Vaccine Advocacy Academy
Mitch Matoga , Fellow, IAS 2024 HIV Vaccine Science Academy
In December 2024, I attended the International AIDS Society (IAS) HIV Vaccine Advocacy Academy, organized by the Global HIV Vaccine Enterprise. What an enlightening experience it was! As someone deeply passionate about the rapidly expanding HIV prevention landscape, I left the academy with a clear picture of where an HIV vaccine fits into the HIV prevention toolbox and why it’s an essential piece for achieving epidemic control.
Now you might be wondering, isn’t it too early to fuss about an HIV vaccine(s)? Absolutely not!
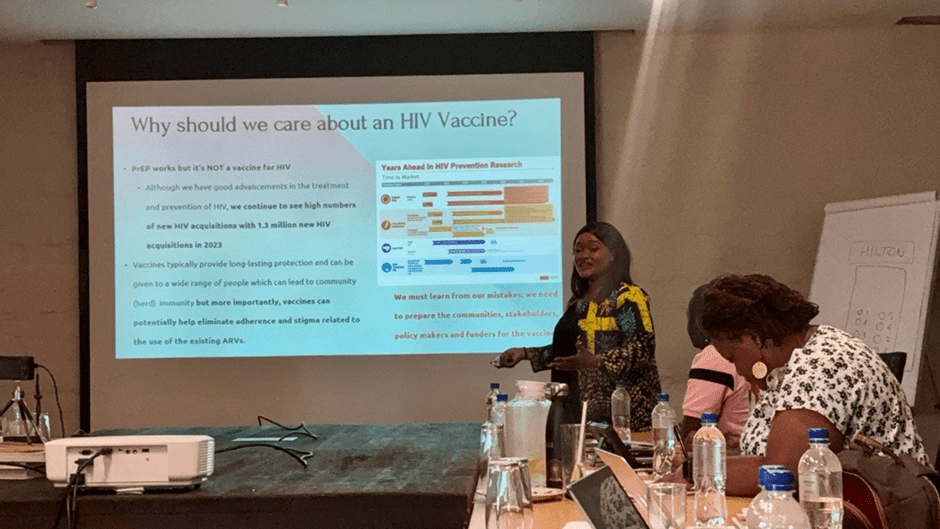
As Roger Tatoud of Origena Consulting said “we need to learn from our mistakes and prepare to ensure the HIV Vaccine is acceptable, accessible and affordable to everyone the moment we confirm efficacy”.
In this blog, I will share insights on HIV vaccine research and development (R&D) in plain English, breaking down the science into bite-sized, understandable pieces — no jargon here!
Why should we care about an HIV Vaccine?
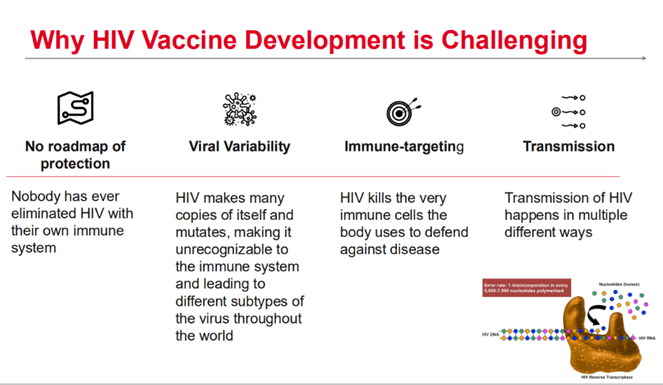
Although we have significant advancements in the treatment and prevention of HIV, we continue to see high numbers of new HIV acquisitions with 1.3 million new HIV acquisitions in 2023. HIV Pre-exposure Prophylaxis (PrEP) works but it’s NOT a vaccine for HIV. PrEP is HIV medicine taken to reduce the chances of HIV acquisition among people who are likely to acquire HIV because of their lifestyle (high risk). While PrEP is an effective prevention strategy targeted at individuals with a high likelihood of acquiring HIV, several challenges limit both access to and uptake of PrEP therefore leaving this group at risk for acquisition. Also, there are still new HIV acquisitions among other groups of people including those classified as “medium or low risk” who are not being targeted for PrEP.
In contrast to a vaccine, the biggest limitation is that PrEP has to be taken regularly (either daily or at intervals such as every 3 or 6 months) which results in adherence challenges. Additionally, the packaging and pills for oral PrEP look similar to ARVs taken for HIV treatment resulting in stigma which is a major challenge that discourages people from starting or continuing PrEP. This is where the vaccine comes in because vaccines typically provide long-lasting protection and can be given to a wide range of people which can lead to community or herd immunity but more importantly, vaccines can potentially help eliminate challenges with adherence and stigma related to the use of the existing ARVs.
“with tailored, accessible services and choice, we may expect better coverage of all people and better coverage of all exposures”
Moses, et al CROI 2024 Abstract #172 : SEARCH STUDY .
A vaccine could be a game changer; however, it should be offered as one of many HIV prevention options not a replacement for existing methods. Using multiple approaches is key to effective HIV control. Studies show that “with tailored, accessible services and choice, we may expect better coverage of all people and better coverage of all exposures” Moses, et al CROI 2024 Abstract #172 : SEARCH STUDY .
What is a vaccine?
A vaccine is a biological preparation that improves the body’s ability to fight off a particular disease (known as immunity). Vaccines work by mimicking what happens during natural infection without causing illness; they use altered versions of viruses or bacteria or other substances to trigger an immune response.

Vaccines are the most effective means of controlling infectious diseases for example, through vaccination smallpox has been eradicated worldwide and polio has been eliminated in some countries. This is because vaccines do not only protect those who use them, they also protect those who do not use them; this is called herd immunity.
What?! I know right.. Let me explain. Herd immunity is a phenomenon where when a significant percentage of the population is vaccinated (protected), it directly reduces the population of people likely to acquire the disease (those not vaccinated) and furthermore indirectly limits the spread of the disease to those not protected (those not vaccinated). Herd immunity protects those who cannot be vaccinated (due to medical reasons, infants, immunocompromised individuals, etc) providing a larger community benefit.
In the long run, vaccines are more cost-saving if distributed widely; by reducing costs that would have gone to providing lifelong treatment and related services.
Advances in HIV Vaccine Research; Promising Strategies
Scientists are currently studying several types of vaccines but because I promised not to bore you with jargons, we’ll focus on Messenger Ribonucleic Acid (mRNA) vaccines and broadly neutralizing antibodies (bNAbs).
Broadly neutralizing antibodies (bNAbs)
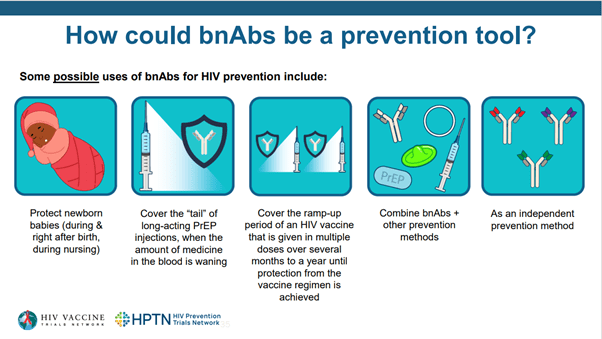
Believe it or not, there are some individuals whose immune systems (specifically their antibodies) block the multiplication of different HIV strains found across the world. Lucky right?! These antibodies are called bNAbs. These individuals have helped scientists understand the behaviour of the body’s immune system against HIV. These antibodies have been harvested by scientists, replicated in larger volumes, and are being studied for potential use as infusions for people at increased risk of HIV infection. bNAbs are likely to offer long-term protection from HIV lasting about 6 months and can be used as an alternative PrEP solution. As you may have guessed, unlike vaccines, bNAbs require repeated administration i.e. every 6 months.
Messenger Ribonucleic Acid (mRNA) vaccines
“mRNA technology has revolutionized the speed and precision of vaccine development”.
Dr. Marianne Mureithi, Kenya AIDS Vaccine Initiative- KAVI
This type of vaccine delivers genetic instructions (mRNA) to cells, prompting them to produce harmless substances (antigens) that resemble ‘the real infection/virus’, which triggers an immune response. mRNA vaccines do not contain live viruses and are quickly broken down by the body, hence they do not cause an infection. They typically require two doses to build strong immunity allowing rapid development and testing. Examples include: COVID-19 vaccines (Pfizer, BioNTech, and Moderna). According to faculty member Dr. Marianne Mureithi (a Microbiologist at the Kenya AIDS Vaccine Initiative- KAVI) “mRNA technology has revolutionized the speed and precision of vaccine development”. Moderna’s mRNA platform is now being applied to HIV and flu vaccines research inspired by COVID-19 mRNA vaccines.
What would an ideal HIV vaccine look like?
Building on lessons learned from vaccine research over the years, an ideal vaccine for HIV should have the following characteristics;
- should stimulate the immune system to produce a response that may help protect against HIV with a few doses
- should provide long-lasting immunity
- should be safe
- should be affordable (and accessible) to all
What is the role of advocates and the community in HIV Vaccine Research and Development?
Get involved, stay informed, and enlighten your circle. Your voice matters!
Advocates and communities—especially people living with or affected by HIV—play a unique role that is critical to the success or failure of any intervention. Decades of experience in the HIV response have shown that interventions are most effective when we “put people first and let the communities lead”.
Here are key ways in which advocates and communities should contribute to HIV vaccine research and development:
- Community Engagement: Fostering trust, ensuring meaningful participation in research, and facilitating informed decision-making.
- Awareness and Education: Combating misinformation, reducing stigma, and promoting accurate information about HIV vaccines.
- Advocacy: Championing policies, securing funding, and pushing for equitable access to vaccines.
- Ethical Oversight: Ensuring research respects community rights, cultural sensitivities, and ethical standards.
- Collaboration: Strengthening partnerships between researchers, policymakers, and affected communities to drive inclusive and impactful solutions.
These roles represent just a fraction of the many ways communities shape HIV vaccine R&D. By centering community voices, we can ensure that scientific advancements are not only innovative but also accessible, ethical, and responsive to the needs of those most affected.
Click here to learn more about HIV vaccine research and development. You can also explore the Global HIV Vaccine Enterprise to get more updates and resources. Get involved, stay informed, and enlighten your circle. Your voice matters!
A special shout out to the International AIDS Society and kudos to the incredible, vibrant, and youthful faculty for such an impactful experience. To my amazing cohort of fellows, it was an honor to learn alongside such brilliant minds. I can’t wait to see the impact we create together.

Leave a reply to Lawrenta Cancel reply